Child ACTT Program Materials
Child ACTT Program Materials
Child ACTT Program Materials — A technology-enabled, family-centered, multidisciplinary community-based treatment for youths 12–18 at risk of residential placement
Overview
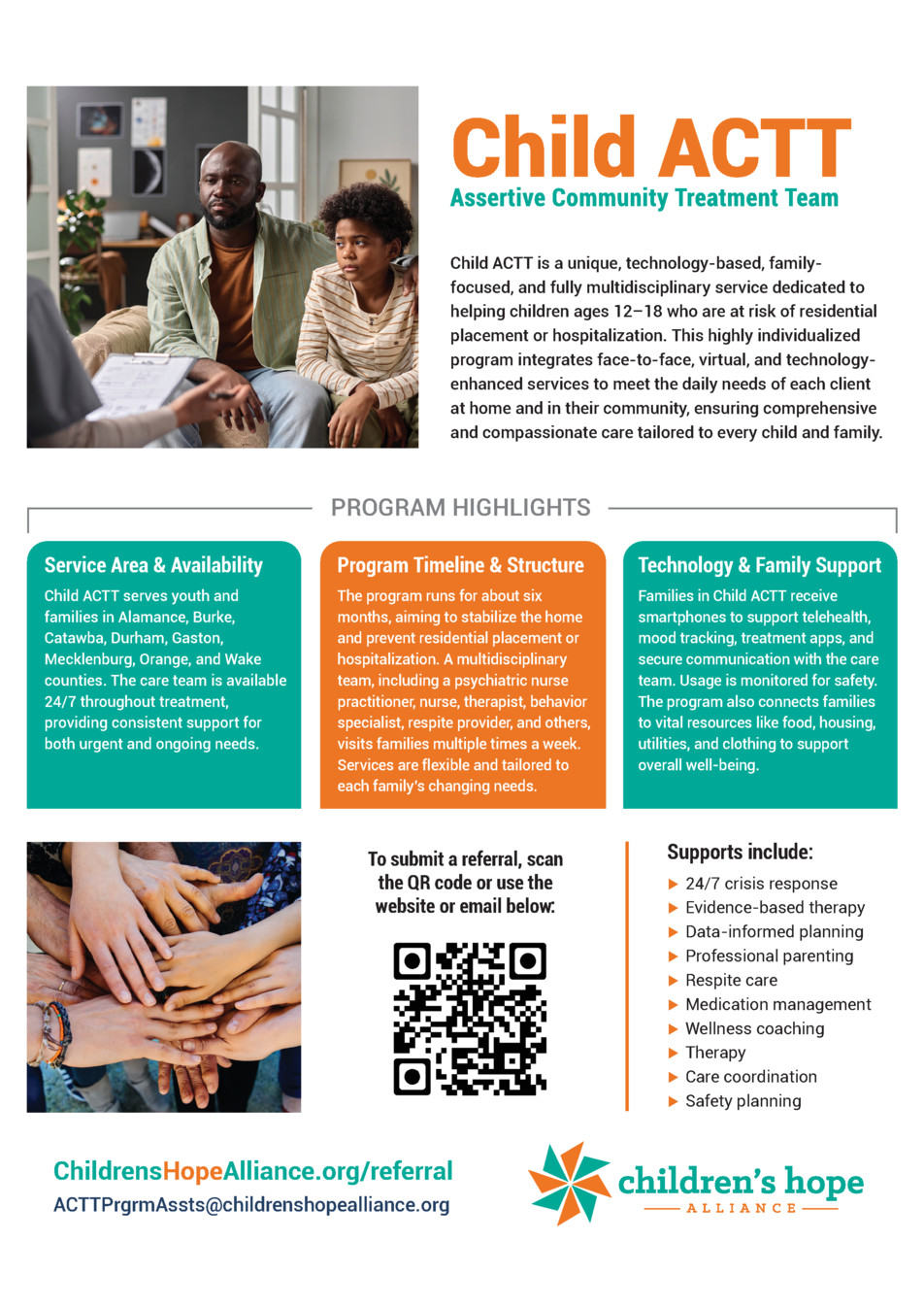
Child ACTT represents a comprehensive, technology-enhanced approach to support young people aged 12 to 18 who face the possibility of being placed in a residential setting or admitted to a hospital due to behavioral or mental health challenges. The program blends face-to-face sessions, remote consultations, and digital tools to address daily needs at home and within the child’s community, ensuring care that is both personalized and compassionate for the child and their family. (Page 1)
Rather than relying on a one-size-fits-all plan, the ACTT model emphasizes customization across medical, behavioral, and social supports, integrating multiple modalities to help stabilize the home environment and reduce the risk of crisis. The aim is to support the child in staying connected with loved ones and familiar surroundings while receiving evidence-informed treatment. (Page 1)
The program operates across a defined service area and is designed to be available around the clock, prioritizing rapid response to urgent needs and ongoing therapeutic support as the child progresses. This integrated framework seeks to foster resilience, safety, and long-term well-being within the family system. (Page 1)
In practice, a diverse team—comprising a psychiatric nurse practitioner, registered nurses, therapists, behavior specialists, respite providers, and other professionals—visits families several times per week. The care plan remains flexible to accommodate shifting family circumstances and evolving treatment goals. (Page 1)
Technology is embedded throughout the experience: families receive smartphones to facilitate telehealth, mood tracking, treatment apps, and secure messaging with the care team. All digital interactions are monitored to ensure safety and appropriate use. (Page 1)
Beyond direct clinical work, ACTT connects families with essential resources—such as food, housing support, utilities assistance, and clothing—to address broader determinants of well-being that can influence mental health and treatment engagement. (Page 2)
For referrals, families or professionals can use a provided QR code, the program website, or the designated email to initiate the process. This streamlined pathway helps connect youth to the most appropriate level of care quickly. (Page 2)
Core supports included in the program range from 24/7 crisis response and evidence-based therapies to data-informed planning, professional parenting guidance, respite care, and coordinated care that centers safety and wellness. (Page 2)
Isabella’s story illustrates how ACTT can transform outcomes. At thirteen, she faced multiple hospitalizations for self-harm and intense anger, with trust and social connections frayed. Her family’s reluctance about medication added a layer of complexity to addressing her emotional and behavioral symptoms. (Page 2)
During early therapy, the clinician concentrated on building trust and providing a safe therapeutic space, recognizing Isabella’s guarded posture and quiet struggles. A pivotal moment occurred when she disclosed self-harming behavior, signaling a turning point in her engagement and willingness to seek support openly. (Page 3)
As trust deepened, Isabella and her therapist crafted a grounding box—an at-home tool filled with comforting items like a teddy bear and a familiar reward system—that helped regulate distress and reinforce motivation. The family’s openness to medication increased, and over time her outbursts diminished while her mood improved. (Page 3)
By the end of her treatment, Isabella’s perspective had shifted markedly. She expressed that the person she had been earlier no longer felt like herself and celebrated progress with meaningful milestones, including stronger connections at school and increased willingness to speak up about bullying. She completed nine months of therapy and returned home with ongoing stability. (Page 3)
Today, Isabella envisions a future with purpose, aspiring to become a veterinarian. Therapy supported her sense of self-worth and equipped her with skills to manage emotions, while hobbies like drawing, listening to music, and spending time with pets continue to contribute to her well-being. (Page 3)
Beyond Isabella’s case, the program emphasizes a shared commitment to community-based treatment that keeps families intact whenever possible. The materials highlight the program’s branding and online presence within Children’s Hope Alliance, underscoring the mission to create solutions when existing resources fall short. (Page 4)
Child ACTT is described as a distinct, science- and technology-driven service that prioritizes the family’s central role and delivers comprehensive multidisciplinary care in the child’s own home and surroundings. The model foregrounds a range of services designed to support physical health, emotional well-being, and social connectedness. (Page 4)
Key service areas are spelled out, including psychiatry and medication management, health and wellness coaching, individual and family therapy, care coordination, crisis management, and enhanced safety planning—each component functioning as part of a coordinated system rather than as isolated interventions. (Page 4)
The program is explicitly designed for children aged 12–18 facing risk of residential placement or hospitalization, with a defined approach to eligibility and service delivery that accommodates diverse circumstances while prioritizing safety and family involvement. (Page 4)
FAQs describe how the team collaborates with external providers when needed, and how safety planning is integrated from the outset. The approach combines daily mood monitoring through digital tools with around-the-clock access to ACTT staff for coaching and crisis support. (Page 4)
Clinical practice within ACTT is grounded in established evidence-based models, allowing clinicians to tailor strategies to each family. Staff training spans multiple modalities, including the Teaching Family Model, Cognitive Behavioral Therapy, Motivational Interviewing, Trauma-Informed Care, and specialized approaches such as TF-CBT, EMDR, and DBT where appropriate. (Page 4)
Safety planning is treated as an ongoing priority, with initial and monthly updates to plans that address potential risks across home, school, and community settings. The service sometimes uses additional measures—such as alarms or secure storage—to mitigate danger while preserving the child’s freedom and family participation. (Page 4)
Even when 24/7 home supervision isn’t feasible, the program emphasizes that parents remain the primary, ongoing supervisors, supported by a responsive ACTT team that can provide guidance and safety coaching as needed. The goal is sustainable safety within the family’s natural environment. (Page 5)
Conversations with families at intake often acknowledge fears about returning home, and the team makes concerted efforts to meet families where they are, reinforcing the tools and supports necessary for a successful transition back to daily life. This includes intensifying services early on and ensuring planned respite to help caregivers manage the adjustment. (Page 5)
The ideal ACTT participant is someone who might otherwise be considered for out-of-home or residential care, with an emphasis on keeping the family together and addressing complex needs through community-based care, rather than moving toward locked or institutional settings. (Page 5)
Eligibility criteria emphasize medical necessity, age range (12–18), a mental health diagnosis, and applicable insurance considerations, with some conditions evaluated on a case-by-case basis to determine the best fit for ACTT versus alternative arrangements. (Page 5)
In terms of data and outcomes, ACTT leverages ongoing assessments and digital mood data to inform clinical decisions and adapt care plans. Regular team meetings ensure that treatment remains aligned with the evolving needs of the child and family. (Page 5)
Referral and authorization processes are straightforward but contingent on safety and insurance, with expedited options available for acute risk and active safety concerns. The process involves a referral form, clinical assessment, and collaboration with the child’s clinical home if needed. (Page 5)
ACTT is positioned as an equivalent service level to residential treatment such as PRTF in terms of goals and intensity, but delivered within the home and community. This arrangement often affords more extensive family therapy, care coordination, and holistic wellness supports that are harder to achieve in a locked setting. (Page 6)
When a child does not respond to ACTT as expected, the team can coordinate alternative services or, in rare cases, arrange a short-term crisis stabilization or hospital stay before reintegrating with ACTT. If a locked, high-security placement becomes necessary, ACTT aids in placement efforts while emphasizing the benefits of community-based care whenever feasible. (Page 6)
Overall, the program underscores a philosophy of shared responsibility among families, communities, and care teams, aiming to keep children connected to their homes and supportive networks. The evidence base cited stresses that well-coordinated community treatment can yield better long-term outcomes than prolonged residential placement. (Page 6)
In sum, Child ACTT embodies a forward-looking, home- and community-centered approach that integrates clinical treatment, family involvement, technology-enabled care, and robust safety planning to help at-risk youths thrive in their familiar environments. The materials emphasize prevention of escalation, prompt crisis support, and a strong commitment to keeping families together wherever possible. (Page 6)